Normal Delivery or C-Section: Pros and Cons
Expectant mothers often find themselves questioning the best mode of childbirth for their baby. Questions like “Will I have a normal delivery or a C-section?”, “Which one is safer?”, and “What is more painful?” are common concerns during pregnancy. In order to make informed decisions, it’s important to understand the pros and cons of both normal delivery and C-section operations.
Here, we’ll explore both approaches, explaining the medical indications for each and discussing their respective advantages and disadvantages.
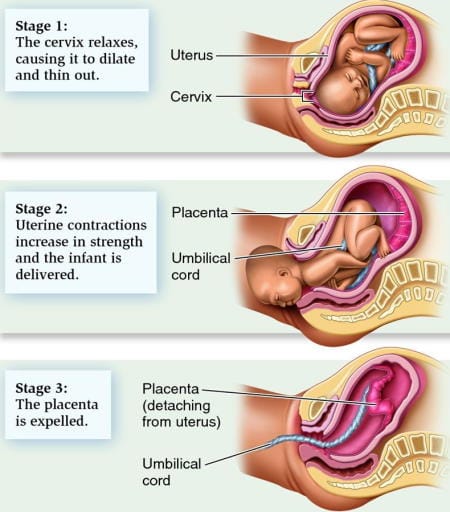
What Is Normal Delivery?
Normal delivery, also referred to as vaginal delivery, is the natural process through which a baby is born via the birth canal without surgical intervention. It is the most common method of childbirth and generally involves less medical intervention compared to a cesarean section.
Vaginal delivery is often the preferred option, given its numerous health benefits for both the mother and baby, provided no complications arise during the pregnancy or labor process.
c section operation, best gynecologist lahore
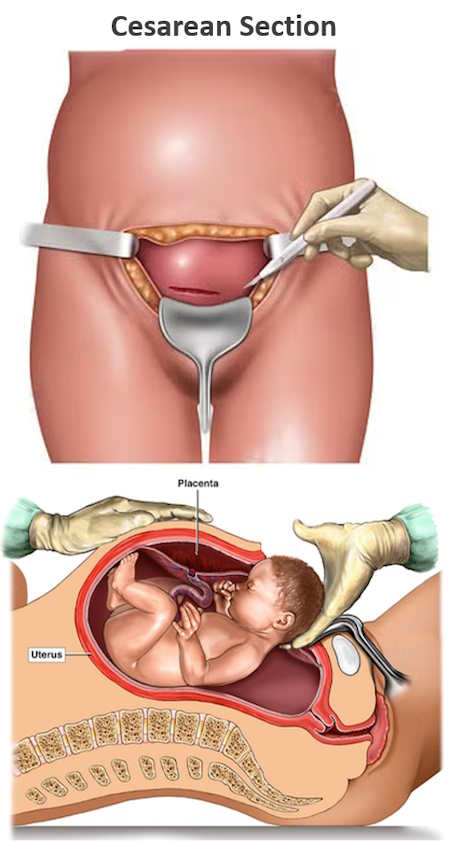
What Is a Cesarean Section and When Is It Required?
A Cesarean section, commonly known as a C-section, is a surgical procedure wherein an incision is made in the mother’s abdominal wall and uterus to deliver the baby. C-sections can either be planned (elective) or performed in an emergency when complications arise during labor. The decision to perform a C-section is based on specific medical factors that make vaginal delivery risky for either the mother or the baby.
Elective Cesarean Section
Elective C-sections are planned ahead of time due to certain medical conditions that may pose risks during vaginal delivery. Some common reasons include:
- Low-Lying / Adherent Placenta: A placenta that is situated in the lower part of the uterus (placenta previa) or on the cervix may risk severe bleeding during vaginal delivery. An adherent placenta (Placenta accreta) may cause severe bleeding and complications requiring cesarean or hysterotomy.
- Fetal Macrosomia: If the baby is significantly larger than average, normal delivery might be difficult, especially if the mother’s pelvis is small.
- Abnormal Fetal Position: Babies in breech (feet-first), transverse, or other unusual positions often necessitate a C-section for safe delivery.
- Previous C-Sections: Women who have had two or more previous C-sections may opt for another one to reduce the risk of uterine rupture during vaginal birth.
- Maternal Infections: Certain infections, like herpes, may prompt a C-section to avoid passing the infection to the baby during vaginal delivery.
- Previous Uterine Surgery: Women with prior uterine surgeries, like myomectomy (fibroid removal), may require a C-section to prevent uterine rupture.
Emergency Cesarean Section
Emergency C-sections are unplanned surgeries performed during labor or delivery due to unforeseen complications. These might include:
- Fetal Distress: Sudden drops in the baby’s heart rate during labor, indicating insufficient oxygen supply, may require immediate intervention.
- Meconium Staining: If the baby passes meconium (stool) in the womb and shows signs of distress, a C-section might be necessary to prevent complications.
- Non-Progressive Labor: If labor stalls and the baby does not move down the birth canal despite efforts, an emergency C-section may be needed.
- Excessive Maternal Bleeding: Severe, unexpected bleeding during labor can be dangerous for both the mother and baby, prompting surgical delivery.
- Severe Preeclampsia or Eclampsia: Pregnancy complications like high blood pressure may require an immediate C-section to ensure the safety of both mother and child.
Normal Delivery vs. C-Section: Pros & Cons
While vaginal delivery is generally safer and has a quicker recovery period, there are certain instances where a C-section is medically necessary. Understanding the advantages and risks of both methods will help expectant mothers make informed decisions in consultation with their healthcare provider.
Normal Delivery: Advantages
- Less Blood Loss: Vaginal births typically involve less blood loss compared to C-sections.
- Faster Recovery: Women who undergo normal deliveries often recover faster and experience fewer complications post-delivery.
- Lower Risk of Infection: Since there are no surgical incisions, the risk of infection is significantly lower in vaginal deliveries.
- Better for Baby: Babies delivered vaginally have an easier time expelling amniotic fluid from their lungs, which helps with breathing. They also benefit from exposure to beneficial bacteria in the birth canal, which supports their immune system.
Potential Disadvantages of Normal Delivery
Although normal delivery has many benefits, there are some potential drawbacks, including:
- Vaginal Tearing: Some women experience tears in the vaginal tissue during childbirth, which may require suturing. While most tears heal without complications, severe tears can lead to longer recovery times.
- Pelvic Floor Weakness: Stretching and tearing can cause muscle weakness, potentially leading to urinary or bowel incontinence.
- Baby’s Nerve or Bone Injuries: In some cases, vaginal births assisted by forceps or vacuum extraction can result in nerve or bone injuries to the baby, though these are typically temporary.
C-Section: Advantages
- Controlled Delivery: C-sections allow for a planned, controlled delivery environment, reducing stress in certain high-risk cases.
- Safety for Complicated Deliveries: For mothers or babies facing complications during pregnancy, C-sections can be life-saving.
- Lower Risk of Birth Trauma: Babies at risk for birth injuries due to difficult vaginal delivery are less likely to experience trauma during a C-section.
- Predictable Timing: Elective C-sections allow for pre-scheduled delivery, which can help with planning for both the mother and healthcare providers.
Risks of C-Sections
As with any surgery, C-sections come with risks. These include:
- Increased risk of infections due to the surgical incision.
- Higher chances of blood clots and hemorrhage.
- Longer recovery times and potential chronic pelvic pain.
- Higher likelihood of complications in future pregnancies, such as placenta previa or uterine rupture.
- Increased risk of breathing difficulties for the baby immediately after birth.
- Potential issues with breastfeeding due to delayed milk production.
How to Increase Chances of a Normal Delivery
For mothers hoping to experience a normal delivery, there are several ways to improve the likelihood of a successful vaginal birth:
- Start Antenatal Care Early: Begin regular check-ups with your healthcare provider as soon as you know you’re pregnant.
- Eat a Balanced Diet: Focus on proper nutrition throughout pregnancy, avoiding excessive weight gain to minimize complications.
- Stay Physically Active: Engage in regular exercise, such as walking or prenatal yoga, to help your body prepare for labor.
- Attend Prenatal Classes: Birthing classes can help you mentally and physically prepare for the experience of childbirth.
- Explore Pain Management Options: Learn about pain relief techniques, including natural breathing exercises or an epidural, to make the delivery process more manageable.
- Develop a Birth Plan: Work with your healthcare provider to create a birth plan that outlines your preferences during labor and delivery.
Vaginal Birth After Cesarean (VBAC)
Many women who have previously undergone a C-section may still be able to have a vaginal birth for future pregnancies. This is known as Vaginal Birth After Cesarean (VBAC). The likelihood of a successful VBAC is higher if:
- The previous C-section involved a low transverse incision.
- The current baby is of average size, and the mother’s pelvis can accommodate vaginal delivery.
- The first C-section was due to a non-recurring issue, such as a breech position.
How to Avoid Unnecessary C-Sections
Many unnecessary C-sections can be prevented through proactive decision-making and supportive strategies. If you are offered a C-section, active participation in your healthcare choices is essential to avoid an unnecessary procedure. Here are several effective strategies to help reduce the likelihood of a C-section while maintaining safety:
- Choose a Provider Wisely: Select a healthcare provider with a low C-section rate, as cesarean rates can vary significantly between practitioners.
- Stay Active: Engage in regular physical activity during pregnancy to prepare your body for the demands of labor.
- Arrange Continuous Support: Consider having continuous labor support from an experienced individual, such as a doula, to assist with comfort measures and labor progression.
- Prioritize Rest: Ensure you get adequate rest in the weeks leading up to your delivery, allowing your body to prepare for the challenges of labor.
- Avoid Induction: Steer clear of labor induction unless it’s medically necessary.
- Delay Hospital Admission: If you plan to give birth in a hospital, collaborate with your provider to delay your admission until active labor begins.
- Stay Upright and Mobile: During labor, remain upright and mobile, ideally with drug-free pain relief methods, and request handheld fetal monitoring to maintain mobility.
- Pain Relief: Discuss with your gynecologist, pain relief options for better tolerability of labor pains like injection, Entonox and Epidural analgesia.
- Explore VBAC Options: If you’ve had a previous C-section, work with a supportive provider and birth setting to explore options for Vaginal Birth After Cesarean (VBAC).
- Breech Position Solutions: If your baby is in a breech or feet-first position toward the end of your pregnancy, discuss options with your doctor or midwife to encourage a head-first position through techniques like external version.
If you are scheduled for a C-section, aim to wait until at least 39 weeks of gestation unless there’s a medical reason for earlier delivery. The final weeks of pregnancy are vital for your baby’s lung, brain, and organ development. Babies born before 39 weeks may face health challenges and require special care.
Trust Your Body and Your Doctor
As you approach childbirth, it’s important to trust both your body and your healthcare provider. Your body is designed for the miraculous process of childbirth, and your doctor is there to ensure a safe and healthy experience for you and your baby.
Conclusion
In summary, the decision between normal delivery and cesarean section should be guided by medical necessity. Normal delivery offers many advantages, including a faster recovery and beneficial effects for the baby. Conversely, C-sections are crucial in cases of medical complications. Prioritize early and comprehensive antenatal care, maintain a healthy lifestyle, and trust your healthcare team to support you in achieving a safe and positive childbirth experience.










