Heavy Menstrual Bleeding ( Menorrhagia ): Causes, Treatment
Many women experience heavy periods, but the cause is not always clear. Conditions such as endometriosis, fibroids, or hormonal imbalances can lead to excessive bleeding. Fortunately, various treatment options, including medications and surgical procedures, can help manage symptoms and improve overall well-being.
How Common Is Heavy Menstrual Bleeding?
Heavy menstrual bleeding is a widespread concern, with nearly one-third of women seeking medical treatment for it. While it may seem common, excessive bleeding is not normal and can significantly impact daily life. In some cases, it may indicate an underlying health issue. If you feel your periods are unusually heavy, it is important to consult an obstetrician-gynecologist (ob-gyn) for evaluation and guidance.
What is Considered Heavy Menstrual Bleeding (Menorrhagia)
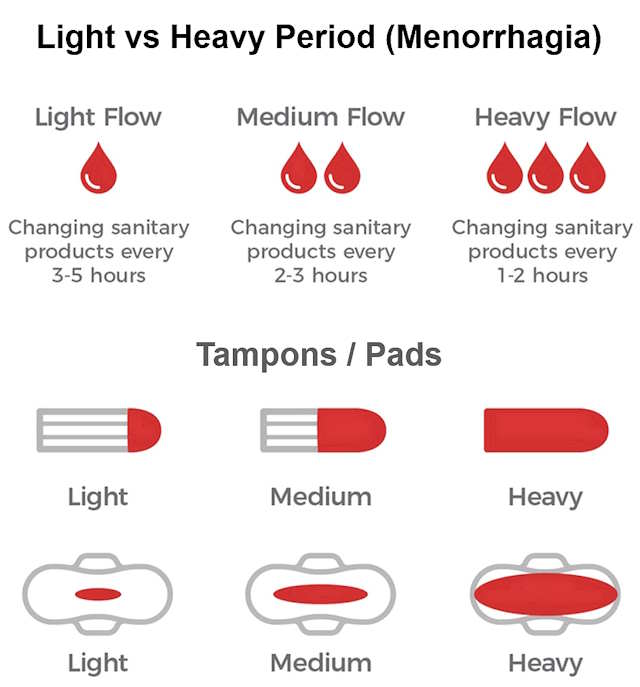
Many women wonder if their period flow is normal or unusually heavy. Since every woman’s experience is different, it can be challenging to know when bleeding becomes excessive. Medical professionals use specific guidelines to determine what qualifies as heavy menstrual bleeding.
What’s Considered a Normal Period?
A healthy menstrual cycle typically:
- Occurs every 21 to 35 days
- Lasts 3 to 7 days (up to 8 days can still be normal)
- Produces 25 to 80 mL of blood (about 5 to 16 teaspoons)
- Requires pad/tampon changes every 3 to 4 hours during heaviest flow
When Is Bleeding Considered Heavy?
You may have menorrhagia (heavy menstrual bleeding) if you experience:
- Losing more than 80 mL of blood per cycle (about half a teacup)
- Bleeding that lasts more than 7 days
- Missing work/school or avoiding activities due to bleeding
- Bleeding through clothes or bedding regularly
- Needing to change protection every 1-2 hours
- Using both tampons and pads simultaneously
- Waking up to change protection at night
- Passing blood clots larger than a quarter
Why It Matters
Heavy periods aren’t just inconvenient – they can:
- Lead to iron deficiency anemia
- Disrupt daily life and activities
- Indicate underlying health conditions
- Cause emotional distress
Common Causes of Heavy Menstrual Bleeding
Heavy menstrual bleeding can be caused by several underlying conditions, ranging from benign growths to hormonal imbalances. However in many cases, heavy menstrual bleeding occurs without any identifiable underlying cause. When no specific abnormality is found, treatment typically focuses on managing the symptoms. The most common causes are listed below:-
Fibroids
Fibroids are abnormal growths that develop within the muscle of the uterus. These non-cancerous tumors affect up to 80% of women at some point in their lives. While many fibroids are small and symptom-free, larger or multiple fibroids can lead to:
- Heavy or prolonged menstrual bleeding
- Pelvic pressure or pain
- Fertility issues or complications during pregnancy
Fibroids vary in size, ranging from microscopic to as large as a grapefruit. Their symptoms often improve after menopause due to declining hormone levels.
Endometriosis and Uterine Polyps
Uterine polyps are small, usually benign growths that form in the endometrial lining or cervix. Symptoms may include:
- Heavy or irregular menstrual bleeding
- Spotting between periods
- Post-intercourse bleeding
While most polyps are harmless, older women may be at a higher risk of developing abnormal changes, making removal advisable.
Endometriosis can also contribute to heavy menstrual bleeding. This condition occurs when tissue similar to the uterine lining grows outside the uterus, leading to inflammation, pain, and in some cases, abnormally heavy or prolonged periods.
Endometrial Hyperplasia and Cancer
Some women develop an abnormally thick uterine lining, a condition known as endometrial hyperplasia. It can cause:
- Heavy or irregular periods
- Blood-stained vaginal discharge
In some cases, this condition may progress to endometrial cancer, which is more common after menopause but can also affect younger women.
Risk Factors for Endometrial Hyperplasia and Cancer
- Age over 45
- Excess body weight (over 90 kg)
- Never having children
- Family history of endometrial, ovarian, or bowel cancer
- Polycystic ovarian syndrome (PCOS)
- Genetic predisposition (e.g., carrying the HNPCC gene)
Adenomyosis
Adenomyosis occurs when endometrial tissue grows into the muscular wall of the uterus, causing enlargement and tenderness. It can lead to:
- Severe menstrual cramps
- Heavy or prolonged periods
- Chronic pelvic pain
Diagnosing adenomyosis can be challenging, as common imaging methods like ultrasound and MRI may not always detect it.
Intrauterine Devices (IUDs)
Intrauterine devices (IUDs) are a popular long-term birth control option, but they can have different effects on menstrual bleeding depending on the type used.
Copper IUDs
- Increased Bleeding: Copper IUDs, such as the Paragard, do not contain hormones and work by creating an inflammatory response in the uterus to prevent pregnancy. However, they often lead to heavier and longer periods, especially in the first few months after insertion.
- Stronger Cramps: Some women experience increased menstrual cramps, which can be more intense than usual.
- Spotting Between Periods: Light bleeding or spotting may occur, particularly during the first six months as the body adjusts.
Hormonal IUDs
- Reduced Menstrual Flow: Hormonal IUDs, such as Mirena, Kyleena, and Skyla, release progestin, which helps thin the uterine lining. This often leads to lighter periods or even complete cessation of menstruation over time.
- Less Cramping: Many women report fewer and milder menstrual cramps compared to their cycles before the IUD.
- Initial Irregular Spotting: In the first few months, some women may experience irregular spotting as their body adjusts to the hormone release.
While IUDs are highly effective, any unusual or prolonged bleeding should be discussed with a healthcare provider to rule out complications such as infection or displacement.
Pelvic Infections
Certain infections can contribute to heavier menstrual bleeding by causing inflammation in the reproductive system:
- Sexually transmitted infections (STIs) like chlamydia or gonorrhea may lead to pelvic inflammatory disease (PID), which can cause heavier or more painful periods.
- Endometritis (infection of the uterine lining) often results from bacterial infections and may cause abnormal bleeding patterns.
- Tuberculosis (rare in most countries) can affect the uterus and lead to heavy menstrual bleeding.
Important note: Pelvic infections often come with other symptoms like unusual discharge, pelvic pain, or fever. If you experience these along with heavy bleeding, see your doctor promptly.
Medications That May Affect Menstrual Flow
Several types of medications can influence your menstrual cycle:
- Blood thinners (anticoagulants like warfarin, heparin, or newer DOACs) reduce clotting ability, potentially leading to heavier or prolonged bleeding.
- Chemotherapy drugs can disrupt normal menstrual cycles, sometimes causing heavier periods before they eventually stop.
- Hormonal medications including certain birth control methods (especially when starting or stopping them) may cause temporary changes in flow.
- Anti-inflammatory drugs like aspirin (when used regularly) can increase bleeding.
- Psychiatric medications such as some antidepressants or antipsychotics occasionally affect menstrual patterns.
If you suspect your medication is affecting your period, don’t stop taking it without consulting your doctor. There may be alternative options or ways to manage the side effects.
Bleeding Disorders
While rare, certain blood clotting disorders can significantly impact menstrual flow:
- Von Willebrand disease (the most common inherited bleeding disorder) affects about 1% of the population. Women with this condition often experience heavy periods from their first menstrual cycle.
- Hemophilia carriers (women who carry the gene for hemophilia) may have heavier bleeding.
- Platelet function disorders or low platelet counts (thrombocytopenia) can prevent proper blood clotting.
Warning signs of a possible bleeding disorder include:
- Heavy periods starting at menarche (first period)
- Family history of bleeding problems
- Frequent nosebleeds (lasting more than 10 minutes)
- Easy bruising (bruises larger than a quarter appearing with minor bumps)
- Prolonged bleeding after dental work or surgeries
Unexplained Heavy Periods
In about 40-50% of cases, no specific cause for heavy menstrual bleeding is found after thorough medical evaluation. This is more common in:
- Women over 35, possibly due to natural hormonal changes as ovarian function begins to fluctuate
- Adolescents in the first few years after starting periods, as cycles regulate
- Women approaching menopause (perimenopause) when cycles become irregular
Even when no cause is found, effective treatments are available. Doctors may recommend:
- Hormonal therapies (birth control pills, IUDs)
- Anti-inflammatory medications to reduce flow
- Iron supplements if anemia develops
- In some cases, minimally invasive procedures
If you experience heavy periods with no clear explanation, keep a detailed menstrual diary tracking flow patterns, symptoms, and how it affects your daily life. This information helps your healthcare provider determine the best management approach.
Occasional Heavy Periods
Occasional heavy periods can result from stress, weight fluctuations, or temporary hormonal shifts. However, persistent heavy bleeding, especially with clots, warrants medical evaluation, particularly for women over 40 (heavy periods after 40 with clots).
When to See a Doctor
You should consult a healthcare provider if:
- Your periods have become consistently heavier over three to four cycles
- Bleeding lasts more than seven days
- You experience severe cramps that interfere with daily activities
- You’re passing large blood clots (larger than a quarter)
- You develop fatigue, dizziness, or paleness (possible signs of anemia)
While occasional variations in menstrual flow are normal, persistent changes in your bleeding pattern warrant medical evaluation. These symptoms may indicate conditions like uterine abnormalities, hormonal imbalances, or other health concerns that require treatment. Even if tests reveal no underlying condition, discussing your symptoms early can help manage heavy menstrual bleeding effectively and improve your quality of life.
How Doctors Diagnose Heavy Menstrual Bleeding
A healthcare provider may start with a pelvic exam to check the cervix and uterus size, though this isn’t always necessary for younger women with typical dysfunctional uterine bleeding. Blood tests to detect anemia are common, as up to two-thirds of women with recurring heavy periods develop iron deficiency from prolonged blood loss.
Additional tests may be recommended if you experience:
- Bleeding between periods or after sex.
- Severe pelvic pain beyond typical cramps.
- Unusual vaginal discharge.
- Symptoms suggesting hormonal disorders (e.g., thyroid issues) or bleeding conditions like von Willebrand disease.
Common Diagnostic Tests for Heavy Periods
- Ultrasound scan: Uses sound waves to detect fibroids, polyps, or structural changes in the uterus. A transvaginal probe may be used for clearer images.
- Vaginal swabs: Checks for infections (e.g., chlamydia) that could cause heavy bleeding.
- Endometrial biopsy: A thin tube collects uterine lining samples to identify abnormalities like cancer or hyperplasia.
- Hysteroscopy: A tiny telescope examines the uterus internally, often with biopsy capability.
- Blood tests: Screens for thyroid dysfunction or clotting disorders.
Tracking Symptoms: The Menstrual Diary
Keeping a detailed record of your cycles helps evaluate symptom severity and treatment effectiveness. Note:
- Number of pads/tampons used daily.
- Days of bleeding and clot size.
- Impact on daily activities (e.g., missed work or social events).
This diary helps your doctor determine if menorrhagia treatment options—such as tranexamic acid for heavy periods or hormonal therapies—are working, as some require several cycles to show full results.
Heavy Menstrual Flow Treatment Options
When dealing with heavy periods (menorrhagia), treatment depends on whether an underlying cause is found. Many women experience heavy menstrual bleeding without any identifiable reason, but effective treatments are still available. Your healthcare provider will discuss the benefits and potential side effects of each option to help you make an informed decision.
Watchful Waiting: When No Treatment Might Be Needed
For some women, heavy periods may not significantly disrupt daily life. If tests reveal no serious underlying condition, you might choose to monitor symptoms without immediate treatment. Regular blood tests can check for anemia, and iron supplements may be recommended if needed.
Levonorgestrel Intrauterine System (LNG-IUS)
One of the most effective treatments for heavy menstrual bleeding, the LNG-IUS (such as Mirena® or Jaydess®) is a small T-shaped device inserted into the uterus. It releases a low dose of the hormone levonorgestrel, which thins the uterine lining. Benefits include:
- Reduces bleeding by up to 90% within 3-6 months
- Often stops periods completely
- Lasts 3-8 years (depending on type)
- Provides highly effective contraception
- Reduces menstrual cramps
The LNG-IUS is particularly suitable for women who want long-term birth control along with relief from heavy periods.
Tranexamic Acid Tablets
For women who prefer not to use hormonal methods, tranexamic acid tablets can reduce blood loss by about 50%. Key points:
- Taken only during your period (typically 3-4 times daily for 3-5 days)
- Works by helping blood clots stay intact in the uterus
- Doesn’t affect cycle length or reduce period pain
- May cause mild stomach upset in some women
Anti-Inflammatory Medications
NSAIDs like ibuprofen, naproxen, or mefenamic acid offer dual benefits:
- Reduce blood loss by about 25%
- Effectively relieve menstrual cramps
- Taken only during menstruation (typically for 3-5 days)
These work by lowering prostaglandin levels in the uterus. Women with stomach ulcers should use them cautiously.
Combined Oral Contraceptive (COC) Pill
The birth control pill is another effective option that can:
- Reduce menstrual bleeding by at least 30%
- Decrease menstrual cramps
- Allow cycle control (can be taken continuously to skip periods)
Modern COC pills are often prescribed for extended cycles (e.g., taking active pills for 9 weeks before a break), which can further reduce the frequency of bleeding episodes.
Progestogen-Based Contraceptives
For women who also need contraception, progestogen-only methods can help manage heavy periods:
- Contraceptive injection: Stops periods in about 50% of women after one year of use
- Contraceptive implant: Often reduces or eliminates menstrual bleeding
- Progestogen-only pill (POP): Typically lightens periods, with many women experiencing no bleeding at all
While not prescribed solely for heavy menstrual bleeding, these options are ideal for women seeking both birth control and period management.
Other Hormonal Treatments
Norethisterone: This progestogen hormone is sometimes used when other treatments fail. Key facts:
- Taken from days 5-26 of the menstrual cycle (not a contraceptive at this dosage)
- Less effective than first-line treatments
- Potential side effects include blood clot risks
- More commonly used as emergency treatment for acute heavy bleeding
Medroxyprogesterone: Often preferred over norethisterone for emergency treatment due to lower risk of complications, though this is an off-label use. When used for emergency control of heavy menstrual bleeding:
- Typically taken 2-3 times daily for up to 10 days
- Bleeding usually stops within 24-48 hours
- Not a long-term solution due to potential side effects
Surgical Options for Menorrhagia
When medications aren’t effective, surgical approaches may be considered:
- Endometrial ablation: Destroys the uterine lining using heat, laser, or energy waves
- Performed through the vagina or abdomen
- Often successful but may need repeating
- Not permanent – lining may regrow
- Hysterectomy: Complete uterus removal
- Considered when all other treatments fail
- Major surgery with longer recovery
- Permanent solution – no future periods
Emergency Treatment for Heavy Menstrual Bleeding
When experiencing dangerously heavy periods, quick medical intervention may be necessary to prevent excessive blood loss and related complications. Here’s what you should know about emergency treatment options.
Medication Options to Stop Heavy Bleeding
For women with sudden, severe menstrual bleeding, doctors may prescribe:
- Progestogen medications (like norethisterone or medroxyprogesterone):
- Work similarly to the body’s natural progesterone hormone
- Help regulate the uterine lining
- Typically taken 2-3 times daily for up to 10 days
- Usually stop bleeding within 1-2 days
Note: While effective, medroxyprogesterone isn’t officially approved for this specific use, though doctors often prescribe it due to its safety profile.
Emergency Room Treatment for Severe Cases
In life-threatening situations, hospital emergency departments may provide:
- High-dose hormone therapy to quickly stop bleeding
- IV fluids to treat dehydration from blood loss
- Blood transfusions if significant anemia develops
- Temporary uterine packing or other procedures to control bleeding
Which Treatment Is Right for Me?
Managing heavy menstrual bleeding can feel overwhelming, especially with so many treatment options available. Choosing the right approach depends on your personal health goals, whether or not you plan to have children, and how severe your symptoms are.
Step 1: Start with Medication
In most cases, the first step in treating heavy periods is medication. Your best option will depend on your plans for pregnancy and overall health needs.
- If you plan to get pregnant soon: Nonsteroidal anti-inflammatory drugs (NSAIDs) or antifibrinolytic medicines may help reduce bleeding. These options can ease symptoms without affecting your fertility. However, they may not be as effective as hormonal treatments.
- If pregnancy is a future goal but not right now: Hormonal options such as birth control pills, progestin-only pills, the hormonal IUD, or a progestin injection can effectively manage heavy bleeding while providing reliable birth control.
- If you do not plan to get pregnant in the future: You can use any of the medical options above. Hormonal birth control methods and antifibrinolytic medicines are often the most effective for reducing heavy bleeding.
Step 2: Consider Surgical Options If Medication Isn’t Enough
If you’ve tried one or more medications and still struggle with heavy menstrual bleeding, it’s time to speak with your health care provider about next steps. In some cases, a surgical procedure may offer longer-term relief.
Final Thoughts
Menorrhagia can significantly impact quality of life, but numerous effective treatments exist – from hormonal options like the LNG-IUS to emergency medications and surgical solutions. While heavy periods are common, they shouldn’t be dismissed as “normal” if they disrupt your daily activities. Tracking your symptoms and working closely with your healthcare provider can help identify the best approach, whether you need how to stop menstrual bleeding immediately during acute episodes or long-term management for heavy periods after 40 with clots. Remember that treatment success may take a few cycles, so patience and consistent follow-up are key.
Frequently Asked Questions
How can I tell if my period is abnormally heavy?
Signs you’re losing too much blood during period include: soaking through pads/tampons hourly for several hours, passing large clots (bigger than a quarter), bleeding longer than 7 days, or experiencing anemia symptoms like fatigue and dizziness.
What’s the fastest way to stop heavy menstrual bleeding?
For immediate relief, tranexamic acid for heavy periods or progestins like norethisterone can reduce bleeding within 24-48 hours. In emergencies, seek medical care for IV medications or other interventions.
Why might my period suddenly be heavier this month?
Occasional heavy periods can result from stress, weight changes, medications, or temporary hormonal fluctuations. However, persistent changes warrant medical evaluation.
Are heavy periods after 40 with clots normal?
While some changes are expected during perimenopause, frequent large clots or dramatically increased flow could indicate fibroids, polyps, or hormonal imbalances requiring evaluation.
When should I go to the ER for heavy menstrual bleeding?
Seek emergency care if you: soak 2+ pads hourly for several hours, feel dizzy/faint, have racing heart rate, or pass palm-sized clots. These suggest dangerous blood loss requiring immediate treatment.
Can I treat heavy periods naturally?
While iron-rich diets and hydration help manage symptoms, most natural approaches don’t significantly reduce blood loss. For clinically heavy flow, medical menorrhagia treatment options are typically more effective.